Section: New Results
Radiotherapy planning
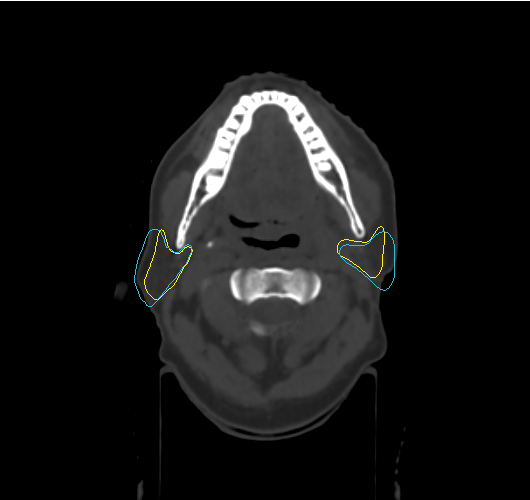
The main challenge of radiotherapy treatment is to irradiate the tumor while sparing the surrounding healthy tissues. In the case of throat cancer, the complexity of the therapy treatment is due to the proximity of organs at risk such as the two parotide glands. The parotide glands are the main salivary glands. An overdose of radiation in these glands may cause xerostomia, which is a medical term for the symptom of dryness in the mouth, or in other words, a lack of saliva. This disease affect significantly the life of the patient: difficulty talking, tasting, chewing, swallowing, excessive thirst, constant pain in the throat etcetera. A radiation therapy treatment of throat cancer takes from 5 to 7 weeks. The treatment is planned several days before the therapy. The planning consist in contouring each organ of the area on CT-scan images and defining the dose of radiation to deliver to each of these organs. This stage is lengthy and takes around two hours per patient. Yet, some anatomical variations occur in the course of the treatment, mainly due to the weight loss of the patients. These variations compromise the safety of the healthy tissues, because the planned treatments is no more up to date. For now, the physicians have no solution goog enough to handle these changes. Xerostomia affects around 20 per-cent of the patients suffering from throat cancer.
The main idea of this work is to create an interface that the physicians could use to redo the planning when it is needed, when the anatomical changes are significant. The purpose is to give to them the possibility to use what they see on images, to recreate the right shape of the contours without recontouring each images, and in a reasonable time. This interface will use their knowledge to determine the new shape of the organs. The work does not aim at providing a fully automatic method because it would reduce its acceptation by the physicians. As the method is based on the input of the physician, they can control the deformation based on images but also on their knowledge.